Is Aspadol 200 mg Safe for Long-Term Use? Risks & Alternatives Explained
Discover the long-term safety of Aspadol 200 mg (tapentadol ER). Learn about side effects, dependency risks, and safer alternatives to ensure effective and responsible chronic pain management.
1. Introduction: Is Long-Term Use Safe?
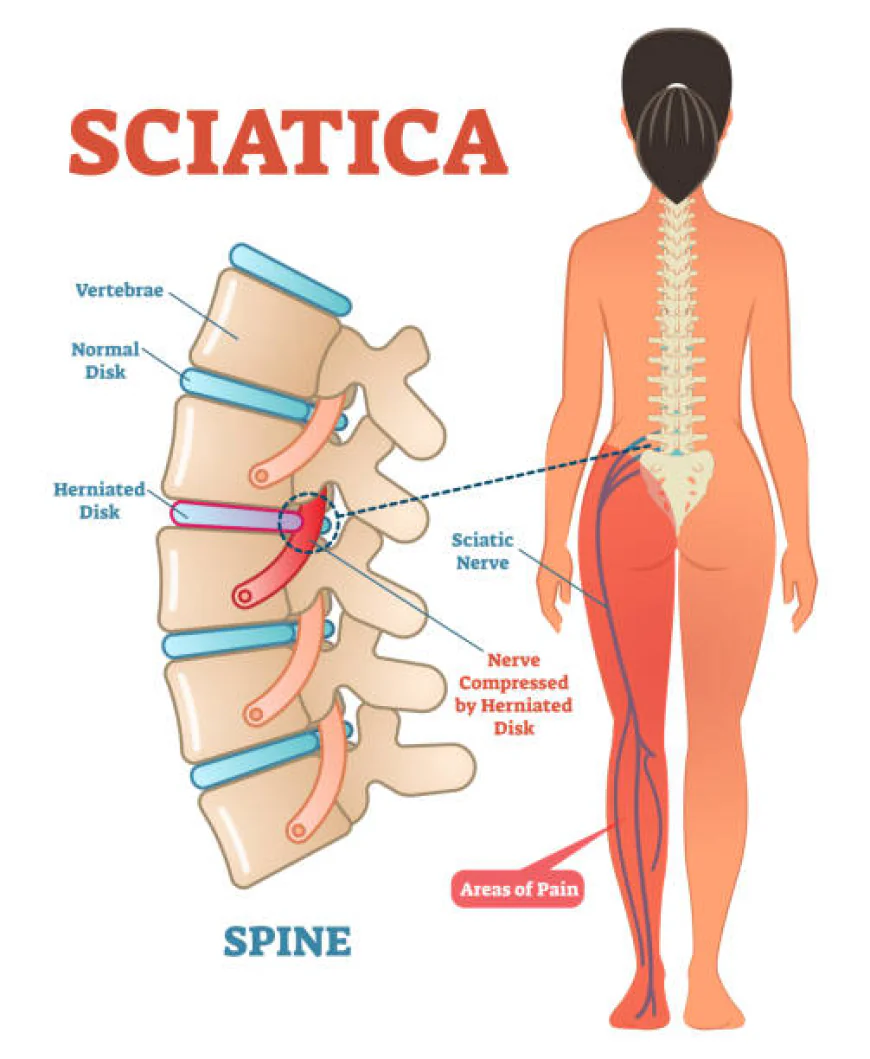
Aspadol 200 mg (tapentadol extended-release) is frequently prescribed to control chronic moderate-to-severe pain—conditions such as low back pain, osteoarthritis, or neuropathic pain. But effective as it is, there is legitimate concern about long-term use—most specifically around side effects, dependence, and health consequences in the long run. In this handbook, we delve into the evidence, highlight risks, and provide safer, evidence-based alternatives.
2. What Science Says About Long-Term Use
2.1 One-Year Clinical Trials
A 1-year randomized trial of tapentadol ER (100–250 mg BID) vs oxycodone CR in osteoarthritis or low back pain demonstrated persistent pain relief (from ~7.6 to ~4.4 NRS) and fewer GI side effects. Discontinuations because of GI problems were 8.6% vs 21.5% with oxycodone .
2.2 Two-Year Follow-Up
An open-label extension established that patients had sustained pain relief (mean NRS ~3.7) and quality-of-life gains at 2 years; the most frequent side effects were nausea (11.8%) and constipation (11.1%).
2.3 Four-Year Tolerability Data
Tapentadol is reportedly well-tolerated long term, even for 4 years, without any unforeseen adverse event. It was less likely to have problems such as serotonin syndrome, hypertension, pulmonary impairment, or convulsions than with traditional opioids.
3. What Are the Long-Term Risks?
3.1 Physical Dependence & Addiction
Tapentadol is highly dependent. Case reports mention extreme tolerance and abuse—e.g., one user built up to 6,000 mg daily over 2 years . Risk of addiction has been established in post-marketing surveillance .
3.2 Tolerance
Increased doses may become necessary over time to get the same relief, increasing the risk of side effects such as constipation and impaired thinking .
3.3 Gastrointestinal & Neurological Effects
Chronic use typically results in constipation, nausea, sedation, dizziness, dry mouth, headaches, and occasional impairment of cognitive function over time .
3.4 Respiratory Depression and Overdose
Particularly with dose escalation or concurrent use with alcohol or sedatives, tapentadol can induce severe respiratory depression—lethal.
3.5 Mood & Cognitive Issues
Depression, anxiety, and memory impairment can be experienced by long-term users. Panic attacks and heart palpitations are reported by Reddit users, even after years of usage.
4. Safer Alternatives for Long-Term Pain Management
4.1 Non-Opioid Medications
-
NSAIDs (e.g., ibuprofen, naproxen)
-
Acetaminophen
-
Antidepressants (TCAs, SNRIs) effective for neuropathic pain
-
Anticonvulsants (gabapentin, pregabalin)
4.2 Non-Pharmacologic Interventions
-
Exercise (walking, swimming, yoga)
-
Physiotherapy
-
Mind–body techniques (CBT, meditation, tai chi)
4.3 Opioid Rotation
Switching to different opioids may maintain pain control and reduce side effects or tolerance issues .
5. Clinical Recommendations for Safe Long-Term Use
-
Regular Risk Assessment – monitor for dependence and misuse behaviors .
-
Use REMS protocols – ensure opioid safety education for prescribers and patients .
-
Lowest Effective Dose – and only as long as needed.
-
Avoid contraindicated combinations – with benzodiazepines, alcohol, sedatives, or SSRIs/SNRIs .
-
Monitor functions – renal, hepatic, neurological, mental health.
-
Plan for tapering – in case of side effects or loss of benefit.
6. Patient Experiences: What Real Users Say
“Been on Palexia IR & SR for roughly 4 years… perfect medication… then started vomiting”— shows that reactions can change with long-term use .
“I take stimulant… heart pounding… doctor shrugged” – signals cardiovascular risks even with long-term opioid use .
“Weird panic attacks after a few weeks” – psychological side effects may emerge even after stable use .
7. Final Takeaway
-
Efficacy: Tapentadol ER can offer effective, long-term chronic pain relief.
-
Better tolerated than traditional opioids—especially in GI side effects.
-
Risks: dependence, tolerance, respiratory issues, mood/cognitive changes.
-
Best Practice: use only when benefits outweigh risks, at lowest effective dose, alongside non-opioid strategies, under strict medical oversight.



 tiza07yeol
tiza07yeol 






