Orthopedic Implants: Restoring Mobility and Quality of Life
Orthopedic implants are medical devices used to support, stabilize, or replace damaged bones and joints. Commonly applied in fracture treatment, joint replacement, and spinal surgeries, these implants help reduce pain, improve mobility, and restore normal movement. Made from biocompatible materials, orthopedic implants play a crucial role in modern orthopedic care and long-term recovery.
The Complete Guide to Orthopedic Implants outlines how the use of orthopedic implants provides benefits to those with musculoskeletal disorders by improving their mobility and overall quality of life. There has been a revolutionary change in the way musculoskeletal care is provided through the use of orthopedic implants. They are created using individualized components that are surgically implanted into the skeletal system to either replace damaged joints/bones or to stabilize/maintain the structural integrity of bone and/or joint systems that have become damaged. The advancements in technology, such as 3D printing, smart materials, and personalized surgical planning, will allow for an increase in the efficiency and durability of orthopedic implants by the year 2026.
Understanding the Fundamentals of an Orthopedic Implant
Orthopedic implants are created from biocompatible (non-immune responding) materials, which will not create a negative reaction from the body once implanted. Therefore, orthopedic implants are considered a major tool for assisting in the restoration of fully functioning bodies of individuals with osteogenesis imperfecta due to trauma or congenital or chronic conditions such as osteoarthritis.
How These Devices Work
The purpose of orthopedic implants is to provide immediate stability to the damaged area of a person's skeletal system. i.e., a broken bone due to a fracture can be stabilized with orthodontics (braces, splints, etc.), and the orthopedic implant used during surgery provides the support to the bone; in joint replacement surgeries, the orthodontic implant will replicate the same size and shape as the joint that is being replaced.
The Biocompatibility Science
Currently, all manufacturers of orthopedic devices are developing innovative methods to create a physical interface between the device and the tissue of the patient’s body. A recent advancement in this field is the use of porous surfaces or special coatings on most orthopedic devices to permit and enhance the biological process of "osseointegration." Osseointegration is the process of allowing bone cells to grow both onto and into the implant. In this way, a permanent biological connection between the patient’s body and the implanted device is accomplished.
Classification of Orthopedic Implant
As a result of the many different types of conditions that fall under the category of orthopedic care, there is no one-size-fits-all solution. The classification of orthopedic devices by engineers and surgeons is based on the clinical function that the implement serves in a patient’s body.
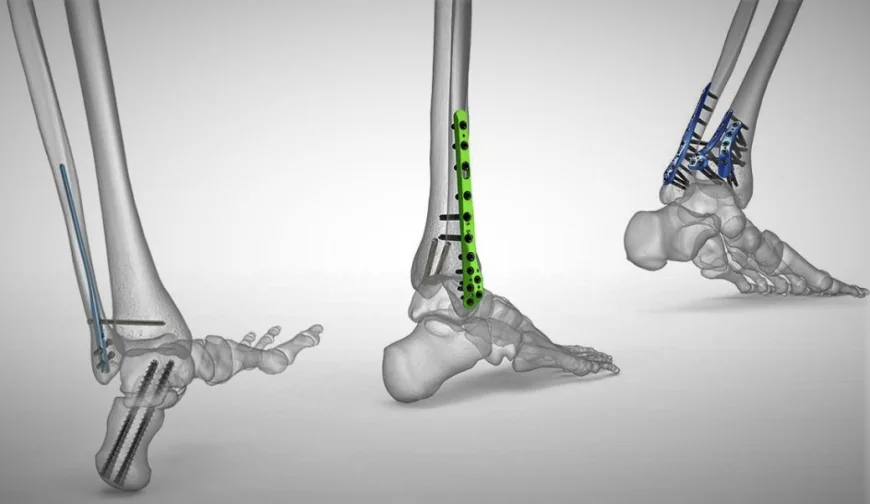
Fracture Fixation Devices
Most fractures require either surgical or non-surgical intervention. Most fractures involving a high degree of displacement or instability usually will require surgery, including the use of one of the following three types of fracture fixation devices.
Plates and Screws:
These devices act as internal splints to hold the fracture in proper alignment.
Intramedullary Nails:
These are long, tubular nails that are placed in the medullary canal of long bones (e.g., femur or tibia) to provide internal support to the bone.
Wires and Pins:
These devices are typically used for smaller bones or in pediatric patients and must take into consideration the growth plate.
Joint Replacement Systems
For patients who have advanced degeneration of their joints, a complete orthopedic implant can be used to replace the damaged joint.
Hip Replacement:
A typical hip replacement consists of a femoral stem, ball, and acetabular cup.
Knee Replacement Systems: Knee replacement systems typically consist of a total resurfacing of the distal end of the femur.
The characteristics of an orthopedic implant
impact the length of time before the implant needs to be replaced and how successful a surgical procedure the orthopedic implant produces. Therefore, a manufacturer has to evaluate the qualities of the material to be used to manufacture an orthopedic implant.
Three areas of consideration will help to determine which materials will provide the orthopedic implant with the appropriate strength, weight, and wear protection or resistance to the patient.
Metallic Alloys
Metals are the standard material for orthopedic implants that bear weight. These three metals provide the greatest strength and weight compared to any other metal for use in the manufacture of a joint replacement. Additionally, these three metals are frequently selected based on the requirements for an individual patient.
Titanium:
Because of its low density (light weight) and the high level of biocompatibility with the human body, titanium is frequently the first choice in joint replacement surgeries. It has a level of elasticity that more closely replicates the elasticity of natural human bone than other metal alloys.
Stainless Steel:
Stainless steel is primarily produced from high-strength carbon steel. When properly manufactured, stainless steel is extremely strong and durable and is typically used to manufacture temporary fixations, such as surgical plates and screws.
Cobalt-Chromium:
Cobalt-chromium is historically used primarily for articulating (or moving) surfaces of knee and hip joints due to its high fatigue and wear resistance.
Advanced Polymers and Ceramics
Polyethylene (PE) is a high-grade plastic that is used to provide a "cushion" effect between two metal components to simulate the function of cartilage.
Polyether Ether Ketone (PEEK):
PEEK is a radiolucent polymer that allows light to pass through it. Surgeons are able to use x-rays to see the bony growth that occurs through the PEEK implant and surgical cage.
Ceramics:
Ceramics are hard and smooth. They reduce friction and the potential for wear-related inflammation to occur in patients with the ceramic implants.
Read more: Best Orthopedic Surgeon in ahmedabad
conclusion
Studies have been completed throughout the years looking at tissue engineering and regenerative medicine, and the line between synthetic orthopedic implants (artificial materials) and bone (natural material) is becoming less of a defined boundary. Future advancements will involve devices that will not only provide a physical means of support but will also assist the body in recovering and healing by supplying the body with growth factors it requires to speed up natural healing.
Frequently Asked Questions
1. What is the normal life of an orthopedic implant?
The life span of the device normally falls between 15 and 25 years. The development of materials, such as high crosslinked polyethylene and ceramic on metal surfaces, will enable some patients to maintain their implant for a lifetime, provided that they care for their implants and health accordingly.
2. Will an orthopedic implant cause metal detectors at the airport to go off?
It depends on what type of metal detector is being used at the airport. High-sensitivity detectors may detect the metal from your hip or knee. For this reason, it is recommended that you inform the security workers and hopefully bring an identification card provided to you by your surgeon for your implant.
3. Is it possible to have an allergy to the materials used in the implant?
There have been rare instances of patients that have been found to be sensitive to metals such as nickel. Your surgeon can make recommendations for alternative materials if you are confirmed to be allergic to metal; for example, your surgeon may suggest a titanium or ceramic implant because they are usually hypoallergenic.
4. If I have an orthopedic implant, can I still have an MRI?
In most cases, the answer is yes. Most modern orthopedic implants are manufactured from non-ferromagnetic metals, such as titanium, and will usually be managed per MRI guidelines. However, you should always inform the MRI technician of your implant prior to the MRI examination.
5. Once the bone has healed, is it necessary that the orthopedic fixations be removed?
The answer depends on the fixation device used. Some fixation devices (e.g., plates and screws) will be used only until the bone is healed. Others (for example, intramedullary nails) are designed to remain in place. Some patients may require removal of their implant due to issues relating to the healing of the bone surrounding the implant.
.










